LEGG PERTHES MESSAGE BOARD |
LEGG PERTHES RELATED LINKS |
|
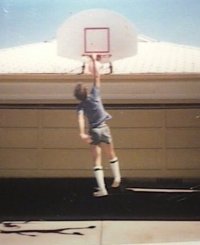
I was 5 or 6 years old here 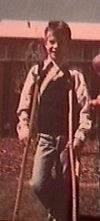 |
It all started when I was 5 years old. I was an active child, I loved to play, and run, and do all the things kids do. One day, when my mother noticed a limp from my hip, I thought nothing of it, denied it all, and just kept being a kid. It was then I began to try walking "normally". I can remember all the doctor visits as if the were just the other day. The biggest impact was when I sat in the ortho's office, with my mom and dad, and the doc told me that I may never walk again......
The news was bad, Leg Perthes, a disease of the hip ball joint. This disease causes the degeneration of the ball of the hip, turning the bone tissue in to a soft, almost liquid form. With any luck, I should be able to walk again in 5 to 10 yrs.....I was very lucky however, The disease was caught very early, and my recovery was of record statistic. Some say they recover in 3 years or less, usually this is because they were not diagnosed at an early stage, usually leading to extreme long term effects.
I can remember, the first few days on the crutches. I didn't want to go to school or any public thing, like scouts, and I didn't even like to get out of bed. My mom would carry me upstairs for breakfast in the mornings, but my dad soon noticed the lack of crutches in the room. I owe him gratitude for getting me started in my "new life". Once I returned to school, my mom would take me to and from, until one day, she didn't show. My father forced her to make me fend for myself, another thing that helped me in my "struggle". That day was the absolute rock-bottom for me, I was left out to dry, the bus had already left.
My story would, in its' own time, become brighter and way more cheerful. In time I was like "SuperTim", Almost everyday someone would say "I can't believe that you can do that !". I remember climbing trees like other kids, playing baseball, racing, and participating in almost every P.E. activity at school. In time, my disability was nearly unnoticed by myself, but I can remember the stares, everyone had to get a look at "the gimp".
Let me explain the "rigging" for my leg. I wore a sling, known as a Perthes sling, I have not seen anything of its kind anywhere on the net, although I hope to have some pics soon. Imagine Miss Universe, the way their geographic location is bannered around their chest. My sling was the same, with a strap that would hang down beneath by bumm. This strap had a lasp, which in turn connected to an eyelet, specially affixed to the heal of my shoe. This kept my leg at about a 110 degree angle, balanced and surely out of the way for any use whatsoever.
The days came and went, one after the other, I became one with my crutches. There were times where I had to fully use one of my arms, like in the hot lunch line. I would use my "bad" leg to hook the crutch of the opposite side, dragging it with me, using my armpit as well. Eventually, I could practically crutch without the use of my arms at all, pit crutching I think I called it. When a person crutches for an extended period, many adaptations come to be. I think this is something never dealt with by a standard broken bone or injury related condition, at least at the same level.
Something about this injury was in fact different. This "disease" came and left me, with little pain felt at any time, with the exception of the work to become a great crutcher. The feeling that everyone was wrong, and this is dream, was a daily thought to me. I felt the lowest of all, thinking I would never be the same Tim again. It was like I was OK, but yet I wasn't able to play anymore, all the kids thought I had a broken leg. I remember people asking me all the time "where's your cast", only to have to try and explain my problem to them.
Soon the time had passed, through the various stages of the Perthes. It was time to prepare to walk again. By now I'm past midpoint of the third grade, having crutched since before first grade started. I was reluctant to believe at first, it wasn't like I could just throw the sticks down and just start running. The first thing was to loose the sling at home, and begin to actually use the leg. I was lucky, my family could afford a pool so that I could rehab frequently in the water. I still, however, had to use the sling at school, or away from home for any reason. My leg was getting stronger, although it was still weak. Eventually I was able to loose the sling at school, within a few months I started riding my bike downhill only, you can imagine what kind of fun that was, but it meant something more to me. At this point all the rehab couldn't happen fast enough for me, I still didn't think I would be the same as I was. Summer came, and I still had to use both crutches, it would become, up to that point, the fight of my life.
I thank the lord, I have been blessed in many ways. Many a time I asked myself, "why me ?". I know today, at over 50 that everyone has there lessons. I know that those 4 years on crutches have helped me in so many other ways.
This pic is from the age of 14 or 15 years
WARNING:
THIS IS NOT OFFICIAL MEDICAL ADVICE, CONSULT YOUR DOCTOR FOR MEDICAL
TREATMENT
My opinion is that non-weight bearing is essential as well as early diagnoses. The hip ball simply softens, the weight crushes the ball ultimately leading to surgery unless action is taken. I know that 3-4 years on crutches seems to be a big deal, but look at the entire picture, believe me, just a short period in a long life. After the crutches and "Perthes Sling", I developed an extremely strong lower body thanks to swimming and bicycling. I even distance ran for a long time, although I don't do that anymore as I'm feeling some arthritis and really want my hip to last. I recently visited my ortho., so far, so good ! :)
LEGG-CALVE-PERTHES DISEASE Legg-Calve-Perthes Disease is a disease that affects the hip bone as it meets the pelvis. This disease, also called Legg's disease, is seen in children, usually between the ages of five and ten. Boys tend to get this disease more frequently than girls, although girls can also develop it. In this disease, the hip bone deteriorates due to decreased circulation to the top of the bone, called the "femoral head." The cause is unknown. The hip joint becomes weak, and is not able to handle any weight. This results in pain in the child's hip or knee. Occasionally, there will be a limp. To diagnose this disease, your healthcare provider needs to do x-ray studies of the hip. Treatment depends primarily on when the problem is diagnosed. The treatment may require bed rest for 6 months to a year, until the condition improves. When the bone can tolerate the child's weight, crutches, braces or casts are usually necessary. Activities can be gradually resumed as tolerated. If treatment is delayed, permanent bone injury may occur and require surgery to replace the hip. Homecare measures that can be used to relieve symptoms include: * heat to relieve pain and * non-prescription pain relievers, such as Tylenol or Motrin An evaluation by a healthcare provider should occur if your child has hip pain, knee pain, stiffness, or a limp.
Here is a brochure offered through the LP Support Group, thanks Barb !
LEG CALVE PERTHES DISEASE
You have been given this brochure because your child has been diagnosed with Leg Calve Perthes disease. Leg Calve Perthes disease is a rare disease of the hip that afflicts approximately 1 in 1200 children. Of those children, only about 1 in four are girls. About 15% of all diagnosed develop the disease in both hips (bi-laterally). Most of these children are very active and often very athletic. The age of diagnosis is usually in between 2 and 12 with the average age of 6. Leg Perthes children tend to be of shorter stature due to delayed bone age. The purpose of this pamphlet is to provide you with information to help you understand the condition and some of the important issues with treatment.
What is Leg Calve Perthes disease?
Leg Calve Perthes disease or LCPD is an osteochondrosis of the hip and is found only in children. It is known by a few other names such as, ischemic necrosis of the hip, coxa plana, osteochondritis, and avascular necrosis of the femoral head. Most commonly it is called Leg Perthes disease or LCPD.
LCPD has an unknown origin. What is known about the condition, is that due to an interruption in blood flow from the femoral artery, bone death occurs in the ball of the hip. As bone death occurs, the ball develops a subchondral fracture. This fracture signals the beginning of bone reabsorption by the body. As bone is slowly absorbed, it is replaced by new tissue and bone.
There are five stages of LCPD: 1) cessation of growth of capital femoral epiphysis - 6 to 12 months in duration; 2) subchondral (or underlying) fracture - 3 to 8 months in duration; 3) reabsorption of bone - 6 to 12 months in duration; 4) reossification (regrowth of new bone) - 6 to 24 months in duration; 5) healed.
Who is at risk?
There is no specific cause known for LCPD, however, there are some risk factors. Some of the factors identified as possible links include obesity, family history, low birth weight, and abnormal presentation at birth. The disease is found more often in Asians, Eskimos, and whites, with a much lower incidence found in Australian aboriginals, American Indians, Polynesians and blacks.
First Symptoms
The first symptoms characterized in LCPD are usually a limp and perhaps pain in the hip, groin or knee (known as referred pain). Often you will first notice limping during your child's active play. They usually cannot tell you of an instance when they hurt themselves. They may not be able to tell you exactly where they hurt, especially if the pain is in the knee area. They may not even experience much pain.
Diagnosis
Initial diagnosis will require an x-ray, magnetic resonance imaging (MRI) or bone scan. Other diagnostic measures may include tests for limitation of abduction, a measurement of the thigh to determine muscle atrophy, and tests to determine the child's range of motion.
Prevention
There is no known effective preventative measure.
Treatment
The Goal The goal of treatment is four-fold: to reduce hip irritability; restore and maintain hip mobility; to prevent the ball from extruding or collapsing; and to regain a spherical femoral head. To reach these goals, the impact of the patient's disease must be determined.
Extent of Disease It is rare for a patient to have whole head involvement. However, age can play an important role in the prognosis of the disease. New bone growth typically reshapes better in younger children and it may continue to improve with growth.
There are several different classifications used to determine severity of disease and prognosis. The Catterall classification specifies four different groups to define radiographic appearance during the period of greatest bone loss.
The Salter-Thomson classification simplifies the Catterall classifications by reducing them down to two groups. Group A (Catterall I, II) which shows that less than 50% of the ball is involved, and Group B (Catterall III, IV) where more than 50% of the ball is involved. Both classifications share the view that if less than 50% of the ball is involved, the prognosis is good, while more than 50% involvement indicates a potentially poor prognosis.
The Herring classification studies the integrity of the lateral pillar of the ball. In Lateral Pillar Group A, there is no loss of height in the lateral 1/3 of the head and little density change. In Lateral Pillar Group B there is a lucency and loss of height of less than 50% of the lateral height. Sometimes the ball is beginning to extrude the socket. In Lateral Pillar Group C there is more than 50% loss of lateral height.
Many doctors utilize these classifications as they provide an accurate method of determining prognosis and help in determining the appropriate form of treatment.
Types of Treatment
Often at the initial diagnosis, the physician may take a "wait and see" approach to get a clearer picture of the progression of the disease. As long as the patient's symptoms are mild, the physician may only prescribe physical therapy exercises to help maintain good range of motion. If the patient's mobility changes, then the physician may prescribe either non-surgical or surgical treatment.
Non-Surgical Treatment
Non-surgical treatments come in varying forms. Crutches are used for non-weight bearing treatment for pain. Casts, traction, and braces help return range of motion and mobility. Range of motion exercises may be given to you by your physical therapist to do with your child in the home.
Surgical Treatment
Tenotomy A tenotomy is surgery that is performed to release an atrophied muscle that has shortened due to limping. Once released, a cast is applied allowing the muscle to regrow to a more natural length. Cast time is about six to eight weeks.
Osteotomy There are different types of osteotomies, and, depending on the need, they are performed at different stages of the disease. At times, with the weakening hip, there is the possibility of the ball slipping out of the socket. To protect it, a femoral varus osteotomy is done. A femoral varus osteotomy, with or without rotation, redirects the ball into the socket.
When the socket of the hip is not giving good enough coverage to help reshape the ball, it may be necessary to have an innominate osteotomy. This osteotomy redirects the socket to cover the femoral head during weight bearing. The shelf arthroplasty gives added coverage of the ball from the top lip of the socket. Both the innominate and the shelf arthroplasty help in reshaping.
Looking to the Future
Studies on long-term results of LCPD indicate that the incidence of late degenerative osteoarthritis is dependent on two factors. Residual femoral head deformity and age at clinical onset are the primary diagnostic factors. If the ball reshapes well and fits well in the socket, arthritis is usually not a concern. If the ball does not reshape well, but the socket's shape still conforms to the ball, the patient will tend to develop mild to moderate arthritis in later adulthood. Patients whose femoral head does not shape well and does not fit well in the socket usually develop degenerative arthritis before the age of 50.
Although Leg Calve Perthes disease cannot be prevented, much has been accomplished toward minimizing its effects. Research and clinical studies continue to provide patients with better long-term results.
A bit more from another source.....
"Perthes' is basically an interruption of the vascular supply to the
growing femoral head," said Dr. Schmidt, professor of orthopedic surgery
at the University of Missouri-Kansas City. The disease generally appears
between the ages of 4 and 8 years and is more common in males than in
females (1 in 800 vs. 1 in 4,000). If untreated, Perthes' disease will
result in a residual deformity of the femoral head, which will flatten and
develop a mushroomlike shape in more severe cases, and may lead to
arthrosis from an incongruent joint, greater trochanteric overgrowth, leg
length discrepancy, and the need for total hip replacement. In one
long-term study, 50% of patients with Perthes' Disease had disabling
osteoarthritis by the time they had reached their sixth decade of life, he
said. It's found more frequently in Japanese, Mongoloid, Eskimo, and
central European children, and infrequently in Australian, American
Indian, Polynesian, or black children, Dr. Schmidt said. The initial
clinical signs are a limp, which is often painless, but can be painful,
and limited hip motion. The hip's internal rotation and abduction will be
limited, while external hip rotation is generally not limited. "Make sure
the pelvis is level when assessing hip motion," he said, noting that one
of the easiest ways to check rotational limitation is to place the child
on his or her stomach. The diagnosis relies upon the anterior-posterior
and frog leg lateral x-rays of the pelvis. Additional x-rays should follow
at 3-4 month intervals to follow the course of the disease and determine
whether intervention is required. Perthes' involves both hips in about 12%
of cases. "In a bilateral hip involvement situation, we also need to do
screening anterior-posterior x-rays of the hand and knee because we want
to look for other conditions that can cause bilateral hip changes, like
epiphyseal dysplasia," Dr. Schmidt said. Clinically, the differential
diagnosis includes transient synovitis, septic arthritis, and
osteomyelitis of the femoral neck. Radiographically, it includes
hypothyroidism, Morquio's syndrome, and multiple epiphyseal dysplasia, he
said. The goal of treatment is to maintain the sphericity of the femoral
head. Doing so will delay and hopefully prevent the onset of degenerative
hip disease in later life. Treatment includes traction, rest,
anti-inflammatory medications, and range of motion exercises. The second
phase of treatment is containment -- keeping the femur in the hip socket.
This can be achieved through an abduction bracing and a variety of
surgeries, including shelf arthroplasty. Shelf arthroplasty offers
immediate containment, improves the situation for later total hip
replacement if needed, and may also stimulate early healing, Dr. Schmidt
said.